Welcome to my Album of Photographs and Memories of Travel, practicing Medicine, culinary Experiments, and other Exploits.
Monday, November 7, 2016
What Internship Looks Like XVIII: Humoralism in Modern Medicine
This graph of descriptive terms in heart failure blew my little history-of-medicine mind in its melding of ancient humoral and modern pharmaceutical medicine.
On the Y axis are body temperatures from "cool" and poorly perfused to "warm" and well perfused. Clinicians check this in their patients by touching their hands and feet to feel the temperature, and maybe pressing down on a nail bed to push out the blood, and then counting how many seconds it takes for the blood to come back after letting go (we call this "capillary refill time," and a good number is less than 3 seconds). If a person's heart is pumping well, then their extremities will have good blood flow and be pink, warm, and with a quick capillary refill. If a person's heart is pumping poorly, then their extremities will be pale, cool, and have a prolonged cap refill, as the body clamps down on peripheral blood vessels to keep most of the blood in the core to nourish the major organs.
On the X axis are relative body-water volumes from "wet" to "dry." A patient is "wet" if their blood is being pumped so poorly that it starts to seep out of the blood vessels into the surrounding tissues: this causes peripheral edema in dependent areas like feet, legs, and buttocks; "crackles" in the lungs; and even bowel-wall edema, leading to poor appetite and slow gastrointestinal transit time. Sometimes these patients have gotten off their usual diuretic, or they have had a "dietary indiscretion" (like Bugle chips, or holiday dinners) such that they have too much salt and/or water on board. A patient who is "dry," by contrast does not have these findings on history or exam.
The symbols inside the graph tell the practitioner what to do: a patient who is "warm and dry" (X marks the spot) is in "compensated" heart failure; their body is balancing poor cardiac output with the needs of peripheral tissues. A patient who is "warm and wet"--well perfused but volume overloaded--should be treated with a diuretic like Lasix (furosemide) to help their kidneys pee out the extra fluid. A patient who is "cool and dry" needs an inotrope to help their heart pump better. But the patient who is "cool and wet" is in trouble indeed, for they have entered a spiral of fluid retention in which the body perceives itself as intravascularly depleted (more water in the tissues than in the blood vessels) and kicks off a cascade of hormones to retain more fluid in the kidneys, which then leaks out into the tissues, and so on in a vicious cycle. These patients are in end-stage heart failure and need a lot of support on the way to heart transplant, or else palliative care and hospice.
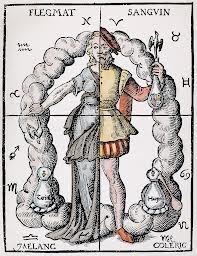
I was tickled when my senior resident drew this graph on the board, because of course I recognized the opposing dyads of warm-cool, wet-dry from ancient Western humoral medicine. Each patient could be described as more or less of each one, although women and younger people were typically assumed to be "wet" (menses, etc.), while men and older people were thought to be "dry" (hence wrinkles). Women were also "cool" compared to men's "hot" tempers and virility. The four humors then named the various combinations: hot and wet was "sanguine" (predominantly blood), hot and dry was "choleric" (yellow bile), cool and dry was "phlegmatic," and cool and wet was "melancholic" (black bile). The result of an imbalance in these internal fluids was disease, and the treatment was its opposite. Was the patient too wet (fluid overloaded)? Dry them out (e.g. bleed them). Were they too cool (lethargic)? Warm them up (e.g. with wine).
Modern physicians do a little of this--in the nineteenth century mainstream practitioners were called "allopaths," meaning they treated disease with drugs that opposed the symptoms, in contrast to "homeopaths," who treat(ed) disease with drugs that reproduce(d) the symptoms. We speed up a slow heart with inotropes or a pacemaker, and we open constricted blood vessels with vasodilators (nitrates for angina). But we also replace hormones that the body no longer produces (as in hypothyroidism or type 1 diabetes), we kill invading microorganisms (as in pneumonia or cellulitis), and we reduce inflammation (with steroid creams, pills, and inhalers). So twenty-first-century clinicians are no longer only or primarily allopaths but could be called "omnnipaths" (all-treaters), or at least "heteropaths" (many-treaters). We see this diversity of approaches in the heart-failure graph, counteracting fluid overload with a drug that dries out the patient, poor cardiac contractility with a drug that improves contraction, and heart failure with surgical options such as LVAD or transplant. However, patients in compensated heart failure get good, old-fashioned life-style advice: stay on your maintenance medications, watch your diet, exercise, and sleep. Even Hippocrates could agree: all things in moderation.
Older
Subscribe to:
Post Comments (Atom)

No comments:
Post a Comment
Your comments let me know that I am not just releasing these thoughts into the Ether...